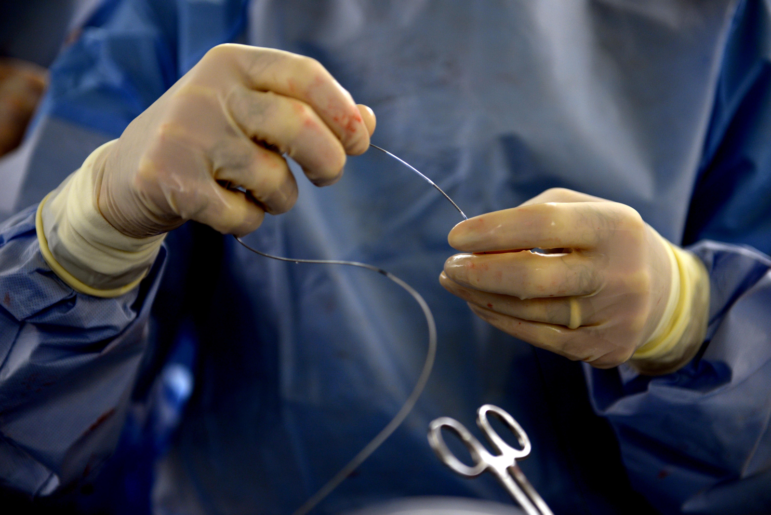
At the American Heart Association annual meeting, the results of the ISCHEMIA trial, the largest study to measure the effect of stents and bypass surgery on patients with stable coronary artery disease (CAD), were revealed.
Stents still not saving lives…
While previous trials have not demonstrated a benefit to invasive approaches for CAD patients overall, researchers have noted that patients with more ischemia (heart artery blockages caused by plaque) seem to benefit more from an invasive approach. Therefore, they wanted to find out whether patients with at least moderate ischemia (higher-risk patients) would experience lower rates of heart attacks and cardiovascular deaths if they received stents and bypass surgery as well as medical therapy.
The study found that for patients with CAD, drug therapy alone was as effective at preventing cardiovascular events and death as drug therapy plus stenting or bypass surgery. Even for patients with severe ischemia, invasive procedures did not reduce the risk of heart attack or death more than drug therapy.
Out of 5,179 participants with stable CAD, 144 patients receiving only medical therapy died while 145 patients in the stent and bypass group died over the course of the trial. The rate of heart attacks was not significantly different between the two groups either; 276 patients in the stent and bypass group had a heart attack, compared with 314 patients taking medication alone.
What would Dr. Lown say?
This study has been hailed as an “extraordinarily important” trial by doctors and the results made waves throughout traditional and social media. However, for doctors like Bernard Lown, who practiced a conservative approach for decades, the ISCHEMIA findings are not groundbreaking.
In 1977, Lown began managing his cardiology patients without a coronary angiogram and subsequent surgeries, going against the standard of practice at the time. The program showed that patients with stable coronary artery disease could be managed with medical treatment, diet, exercise, and stress management rather than surgery, without increasing mortality. Over the next twenty years, Lown’s group continued to manage most of their patients (many of whom had been told by other doctors that they needed surgery) with medical therapy and lifestyle changes alone, with successful results.
Since the early 1980s, many trials have shown that stents do not improve rates of mortality or heart attacks more than medical therapy alone for patients with stable CAD. And yet, invasive cardiac procedures are still common for patients with stable CAD. Why?
Lown’s method and the ISCHEMIA findings go against the intuitive idea that arteries with plaque are like a “clogged pipe,” and that opening blocked arteries prevents heart attacks and death. In fact, opening up an artery only treats the symptom of the disease; plaque buildup in the arteries is best ameliorated with lifestyle changes and medical therapy.
As Louisville cardiologist Dr. John Mandrola writes about the trial in Medscape, it is hard to disabuse the clogged pipe analogy because it fits so well with how we believe our bodies should work. “While part of our brains can understand the data, another part of our brain cannot unsee the gnarliness of a severely stenosed coronary artery,” he writes.
Changing hearts and minds?
Will ISCHEMIA be the trial that changes the standard of care for stable CAD? There’s some hope, as the results may soon be incorporated into AHA guidelines. However, as Dr. Vikas Saini said in an Axios interview, “Established practices die hard, especially when there is a substantial culture, mindset and financial structure reinforcing that behavior.” It’s easy to see how doctors could justify still doing invasive procedures for patients who don’t need them, despite the clear findings of the trial. For example, at the AHA conference, the “headline” of ISCHEMIA was that stenting shows a benefit for angina symptoms, although we do not know that for sure until we compare stenting to a sham procedure (spoiler alert: there isn’t a benefit).
Headline at #AHA19 contrasts with take home from major newspapers… AHA portraying #ISCHEMIA as positive: ‘Early intervention vs conservative therapy can improve angina symptoms…’ Interesting. Not the main finding in my view. pic.twitter.com/s7SP5By3mY
— Harlan Krumholz (@hmkyale) November 17, 2019
Maybe a more important question is, was the ISCHEMIA trial worth it? More research to build the case for appropriate cardiology care is always welcome. However, the trial cost $100 million of public funding, which is no small sum. “It’s sort of like a $100 million government study to prove that climate change is real,” said Saini. However, if Dr. Lown’s method of using medical therapy for stable CAD rather than invasive procedures becomes the standard of care, it will save the health care system an estimated $500 million each year, and avert potential harm from invasive procedures for thousands of patients as well. If the results of the trial finally stick, ISCHEMIA will have been a good investment.