VIDEO: Racism and Hospitals
Lown Presents is a series of virtual events that provides a deep dive into topics at the intersection of health policy, health equity, and high-value care. View all events in the Lown Presents series!
How does structural racism manifest in the hospital sector and what can we do about it? At the first in the Lown Presents virtual event series, Dr. Vikas Saini and Shannon Brownlee were joined by Dr. Mary T. Bassett, Director of the FXB Center for Health and Human Rights at the Harvard School of Public Health, and Milton R. Nuñez, CEO of NYC Health + Hospitals/ Lincoln to discuss this critical issue. Watch the full video of the event above!
What do we mean when we talk about racism in health care?
Brownlee and Saini first set the stage for the discussion by giving some key examples of racism impacting health care. When Saini moved from Canada to New York City in the 1970s and took a job as a cab driver, he had an enlightening experience about race in America. As he was driving around the city, he noticed dramatic differences in racial demographics of neighborhoods just a few miles away. Although New York City had no laws mandating apartheid like South Africa, the market itself was effective at segregating the city. This residential segregation remains, and continues to impact health disparities, since the environmental, economic, and social conditions of where we grow up shapes our health more than our genetics. One can see just by looking at differences in life expectancies across neighborhoods how strong the connection between location and health can be.

Brownlee shared some current headlines about structural racism and health, pointing out enormous racial disparities in Covid-19 burden. The latest information from the Centers for Disease Control and Prevention shows that from May-August, 24% of those who died from Covid-19 were Hispanic or Latinx and 19% were Black. Within the entire US population, 18% of Americans are Latinx and 12.5% are Black.

Diving deeper into the impact of racism in hospitals, Bassett shared some recent research on how Black patients are treated differently in the hospital from white patients. Bassett noted that erroneous ideas about biological differences between Black and white people that date back to the era of slavery (Black people are less sensitive to pain and heat, for example) still impact clinical care today. Not only do Black adults experience more pain before they get medicated, Black children also are given pain medications later than white patients.
A large part of the outsized burden of Covid-19 on people of color is because of conditions that were created long before the pandemic, said Bassett. Workers have become increasingly vulnerable, unionization has declined, affordable and safe housing is increasingly unavailable, and as health care costs have risen, many people are still uninsured and underinsured.
Nuñez explained how structural racism impacts the community he serves. Overall, the Bronx is ranked dead last in health outcomes among NYC neighborhoods. The majority Black and Hispanic community deals with health issues such as obesity, heart disease, asthma, substance abuse, and mental health challenges.
But the most obvious manifestation of racism is access to health care. “We have one primary care doctor for every 2000 residents in the South Bronx. Across the river in Manhattan, it’s one doctor for 730 residents,” said Nuñez.
“If you don’t have primary care, then access to specialty services and clinical trials is even more daunting. The gap in access is already baked in.”
Milton Nuñez, CEO of Lincoln Hospital
Lincoln hospital works hard to recruit primary care doctors and dentists but often clinicians choose to practice elsewhere rather than in their community, leading to a shortage of providers.
What does the Lown Index show about structural racism and hospitals?
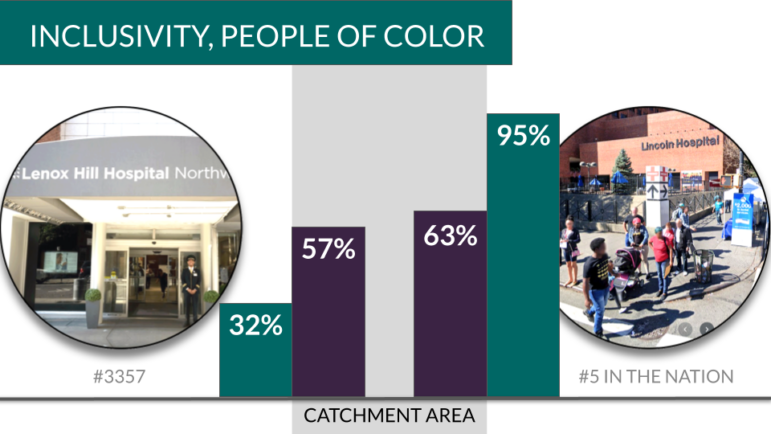
One of the fundamental findings on the Lown Index was that hospitals in the same city — within communities that have similar demographics– often serve very different patient populations. For examples, Lincoln hospital was ranked the most inclusive hospital on the Lown Index. About 95% of their Medicare patient population is non-white, and their average Medicare patient income is $28,000.
Only 22 minutes away by subway, Lenox Hill hospital in Manhattan ranks far lower on inclusivity. Only 32% of their Medicare patient population is non-white, and their average Medicare patient income is $72,000.
Why does Lincoln serve so many more people of color and low-income patients than Lenox Hill? Nuñez says it’s because Lincoln Hospital focuses on serving their immediate community. Their staff resembles their patient population and many staff members live in the South Bronx. Lincoln Hospital also has a community advisory board that holds the hospital accountable for serving their community. “If more hospitals took this approach, the patient base that they served would reflect the community that they serve,” he said.
“We’re never going to be the facility advertising everywhere to get patients from Westchester or Brooklyn.”
Milton Nuñez, CEO of Lincoln Hospital
Bassett noted that our health care delivery system is fragmented, divided between public and private. Despite their nonprofit designation, most private nonprofit hospitals are still driven by profit. Private hospitals may cherry-pick wealthier patients with private insurance and avoid taking patients with public insurance, funneling poorer and sicker patients to the public hospitals. “The public sector valiantly serves its community but its underresourced. This would be much helped if we had a single-payer system,” said Bassett.
Patient choice also makes a difference, because people feel safer at a hospital knowing there are clinicians and staff who look like them. Bassett told a story about how as a medical student, she caught her fellow students practicing a procedure that they didn’t know how to do on a Black patient. She stopped them right as they were preparing to put a needle in the patient’s chest.
“This is a consequence of being in a society where Black and Brown bodies are undervalued.”
Dr. Mary T. Bassett, Director, FXB Center for Health and Human Rights
Nuñez agreed, pointing out that people in his community wouldn’t be sure that a hospital like Lenox Hill would accept their insurance. Even if they did, there’s still an issue of whether they would feel comfortable in an institution where there are very few Black or Latinx clinicians.
What can hospitals and medical schools do to advance equity within their walls?
Participants stressed community accountability as key to reducing disparities in access. More hospitals need community representation on their board and within their governing bodies, said Nuñez. Other things hospitals can do to fight racism within their walls is recognize and work on unconscious bias with staff.
“If you’re going to solve an issue, we have to be honest and upfront about it.”
Milton Nuñez, CEO of Lincoln Hospital
Medical training that bases clinical care on so-called “biological” differences between races also needs to be changed. Bassett gave the example of a spirometer, which tests for asthma, having a different setting for white and Black patients, assuming that lung capacity for Black people is worse. Medical students are still taught that disparities are intrinsic in being black, which propagates the idea that “these patients are patients we can’t look after, they are too sick, they will never be as healthy,” said Bassett. “This is pure and simple racism.”
Medical schools also have to make a commitment to recruiting and supporting students of color, and creating a residency pipeline from which hospitals can hire. “It’s an act of will on the part of medical schools to increase their enrollment [of black students],” said Bassett.
“The number of Black men in medical school is about the same now as it was in the 1970s.”
Dr. Mary T. Bassett, Director, FXB Center for Health and Human Rights
What can individual clinicians do to combat racism in health care?
Many audience members wanted to know — what could they do to fight racism at their institutions? One good way is to stand up for Black lives as a member of the hospital. Nuñez said that one of the proudest moments for him was seeing their residents and medical staff rally with the community this summer and demonstrate with them. “They helped to lead the charge, so our voice was heard loud and clear with the community,” he said.
Within the hospital itself, examining one’s biases and talking about these issues with colleagues is key. If a patient comes in who is intoxicated or homeless, it’s easy for clinicians to write them off or even disrespect them. Clinicians have to remember that every patient who comes in is a person with a family, a past, and a future, said Nuñez.
What policies do we need to tackle structural racism in health care?
Having a single-payer system that paid hospitals the same reimbursement rates for all patients could go a long way toward reducing gaps in access, since many hospitals currently exclude patients with private insurance. It would also boost resources for underfunded safety net hospitals. For example, if Lincoln Hospital got paid Medicare rates for all of their patients, they could expand care, offer more specialty services, and reduce wait times significantly, said Nuñez.
Federal and state regulators could also strengthen the community benefit requirement for nonprofit hospitals. Hospitals don’t just provide medical care, they are major players in finance and real estate. Should hospitals that turn their buildings into condos still be given nonprofit status? Is it a good idea for hospitals that own multiple buildings in a community–not all directly related to delivering health care services– to not pay property taxes on these buildings? These questions are worth considering more closely.
Measuring what matters
The Lown Hospitals Index is an important first step toward measuring everything that matters for hospitals, but there are many other potential data points as well: gender gaps in payment among hospital executives, living wages for all staff, number of lawsuits against patients for medical bills, and more.
Nuñez suggested creating incentives for hospitals to opt into reporting these kinds of metrics. When the Leapfrog survey of patient safety first came out, hospitals did not want to participate. But now hospitals have opted into this voluntary reporting, because the alternative of not reporting raises more questions about their safety metrics. “Peer pressure is a great way to get folks to move,” said Nuñez.
Bassett was hopeful that this moment will carry forward into real action on the part of hospitals. “I haven’t seen an attention to the enduring impact of racism on medicine as I’ve seen in the past few months. I’m very hopeful that attention won’t shift,” she said.
