Despite efforts to expand access, disparities in healthcare use are wider than ever
How have racial disparities in the use of healthcare services changed since the Civil Rights movement in the early 1960s? Despite policies to expand healthcare access, racial disparities in how much healthcare people have actually widened over the past six decades, a recent study in JAMA Network Open finds.
Researchers from Texas Policy Evaluation Project, Harvard Medical School, and the Harvard T.H. Chan School of Public Health analyzed 29 nationally representative surveys of health care use and expenditures to find out how gaps between Black and white Americans changed between 1963 and 2019.
Their measures of healthcare utilization included: The number of doctor, dentist, and emergency department visits per year; how many days spent in the hospital per year; and total healthcare spending.
They found that racial gaps in the number of doctor’s visits per year and total health spending narrowed slightly in the 1960s and 70s. This may be a result of the 1964 Civil Rights Act, which made racial segregation and discrimination based on race illegal, and implementation of Medicare and Medicaid in 1965, which expanded access to healthcare and forced hospitals to desegregate to gain federal funding.
Yet these trends did not hold. Starting in the early 80s, these gaps widened, even throughout the implementation of the Affordable Care Act in the 2010s. From 2014-2019, Black people had 2.63 fewer ambulatory care visits per year, 0.52 fewer dental visits, and $992 lower total health expenditures than white people. These patterns were only partially explained by differences in income and insurance type, the researchers found. Emergency department visits and inpatient days were slightly higher for Black Americans, but these patterns were largely due to differences in socioeconomic status.
“The White-Black gap in expenditures is at an all-time high, and disparities in ambulatory care visit rates are larger today than in 1963.”
Dickman et al., JAMA Network Open
The authors point out that the 1980s brought several economic and social policies that may have lessened healthcare access for Black Americans such as reduced enforcement of civil rights laws, skyrocketing incarceration of Black men, and stagnating Medicaid enrollment.
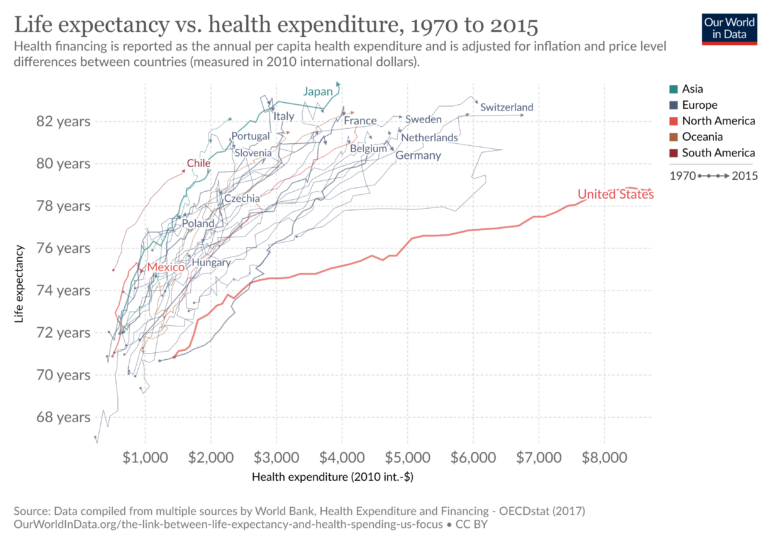
This period also coincides with significant deregulation in the healthcare space, an increase in private insurance and for-profit hospitals, and higher administrative costs in healthcare. It was around this time that the relationship between healthcare spending in the US became divorced from actual health gains, making it an outlier among wealthy countries.
This study is more evidence that racism in healthcare access is persistent and structural — it’s baked into our institutions and very difficult to remove. Part of the issue is that our hospitals are still “separate and unequal.” The Lown Institute Hospitals Index found that de facto racial segregation is still prevalent in hospital systems of major US cities, likely driven by differences in insurance type (hospitals make more money caring for privately insured patients, who are more likely to be white) and historical patterns of residential segregation. Many of the hospitals serving communities of color are under-resourced and have lower quality of care.
Existing policies have not been enough to combat these long-standing issues. Even with the Affordable Care Act, Black Americans are more likely to report not having a regular primary care provider than whites. Cost still plays a significant role in healthcare disparities; Black Americans are 65% more likely to avoid care due to cost, and are 50% more likely to have medical debt compared to white Americans.
The JAMA study authors point to other factors that make it less likely Black Americans will seek care, such as “household wealth, residential and occupational segregation, inadequate transportation, inability to take time off from work…differences in cultural norms, and patients’ beliefs that they may be unwelcome, will face bias, or cannot trust the health care system.”
Clearly we need larger steps to expand access to care for all. Universal health coverage that reimburses doctors similarly for public and privately insured patients would go a long way to reducing disparities. The JAMA study authors also recommend more training of Black healthcare professionals and investments in Black-serving health facilities, to improve trust between doctors and patients, and build capacity at institutions already serving communities of color.
