Where is the evidence for common orthopedic procedures?
Orthopedic procedures — procedures related to bones and muscles like knee and hip replacements, spinal fusion, and ligament repair– are incredibly common. An estimated 22 million orthopedic procedures were performed worldwide in 2017, and this number is only expected to grow.
As these surgeries have become more prevalent, researchers are taking a closer look at the evidence behind them. Although orthopedic surgeries have the potential to reduce pain and improve mobility, they are among the most costly and come with risks of complications.
In a recent analysis in The BMJ, professor Ashley Blom at the National Institute for Health Research in the UK and colleagues looked extensively at the evidence behind ten of the most common orthopedic procedures. In particular, they wanted to find out what results randomized controlled trials (RCTs) show for these procedures, as RCTs are the gold standard for evaluating the clinical effectiveness of an intervention. Randomizing treatment groups is key to neutralizing the placebo effect of medical procedures. As we have seen from RCTs of stents, vertebroplasty, shoulder arthroscopy, and others, even common procedures thought to be effective may not stand up to the rigorous test of randomization.
Blom and colleagues found that when focusing on RCT data, only two of the ten orthopedic procedures (carpal tunnel decompression and knee replacement) were superior to medications or physical therapy (non-surgical treatment). For two procedures (hip replacement and arthroscopic meniscal repair), there were no RCTs comparing these surgeries to a placebo or non-surgical treatment. For all the other procedures studied, RCT data showed no difference on measures of disability or function compared to non-surgical care.
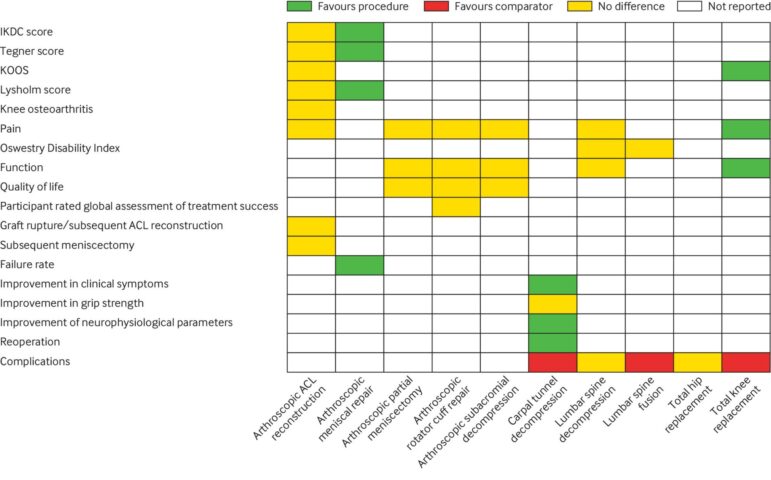
“Although they may be effective overall or in certain subgroups, no strong, high quality evidence base shows that many commonly performed elective orthopedic procedures are more effective than non-operative alternatives,” the authors write. Yet, some of these procedures are recommended in national guidelines.
This study opens up a necessary conversation about what kind of evidence we accept as enough to adopt a new standard of care. Should we encode procedures within guidelines if they haven’t shown to be better than non-surgical treatment? Given how often we see medical reversals after RCTs are conducted, the gap in evidence for certain orthopedic procedures means that we don’t really know if they work — and there may be a reckoning later when we finally do the trials.
