No evidence for common bladder pain treatments, patient advocates find
Interstitial cystitis or painful bladder syndrome (IC/PBS) is a broad diagnosis that encompasses urinary urgency, frequency, and pelvic pain. Although bladder pain and urgency is relatively common, affecting as many as 500,000 people in the U.S. each year, there is no definitive “cause” of IC/PBS. Rather, these symptoms may be caused by several factors, including infection, inflammation, stress, pelvic floor dysfunction, dietary issues, and more.
However, the inability of some doctors to see “beyond the bladder” and investigate the underlying causes of bladder pain and urgency has led to an increasing use of invasive procedures, which have little evidence of benefit and can be harmful.
What treatments are recommended for IC/PBS?
According to the American Urological Association guidelines, the first courses of treatment for most chronic bladder pain patients should be behavioral changes (such as diet and smoking) and stress management. Physical therapy, pain management, and oral medications are listed as second-line treatments. If these do not work, the AUA lists more invasive procedures such as hyrodistention (stretching the bladder with water), botox injections, and medications injected into the bladder through a catheter.
The guideline notes that invasive procedures have little evidence to support their benefit, giving them an Evidence Grade C (recommended based on observational studies that are inconsistent, have small sample sizes, or have other problems that potentially confound interpretation of data).
Very few randomized controlled trials have been conducted for treatments commonly given to IC/PBS patients, despite these treatments being used for decades and having serious potential side effects. Regarding the overall quality of evidence on IC/PBS treatments, these Swedish researchers wrote:
“Many studies have poor descriptions of patients or are of a pilot character, with no follow-up by larger trials. Controlled studies are rather scarce. On the other hand, some good-quality studies following up positive pilot trials end up with negative results.”
Urologist Priyanka Gupta at Beaumont Health System in Michigan and colleagues put it more bluntly in a 2015 paper, writing that “Over 20 years of bladder directed therapy for IC/BPS sponsored by both industry and the National Institutes of Health (NIH) has shown no treatment to be superior to placebo.”
Increasingly, doctors are recognizing that bladder pain and urgency is often a symptom of a larger problem with many potential causes, and that we need significant proof that “bladder directed” therapy works. But has this recognition translated into change of practice?
What treatments are patients given?
Although the AUA guideline recommends conservative treatment options first, research by patient advocates shows that many patients are getting invasive procedures for bladder pain. This is concerning because there is little evidence to show that patients benefit from these procedures, and they can have serious side effects such as chronic pain, bleeding, and antibiotic overuse. Repeated antibiotic use especially can lead to irreparable damage to the microbiome, which can lead to fungal infections like candidiasis, and–ironically–more urinary problems.*
Kay Zakariasen, a former IC/PBS patient and patient advocate, worked with Dr. Jennifer Hill, a urologist at Lenox Hill Hospital, to develop, administer, and publish a survey of a sample of patients who sought treatment for IC/PBS. They wanted to know which treatments patients were being given, and how patients perceived the benefit or harm of these treatments.
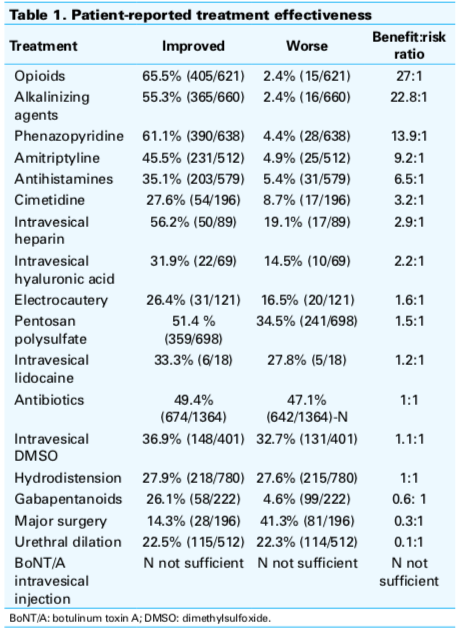
They found that, despite the lack of evidence for invasive treatments, many patients had received invasive procedures. More than 60% of patients had hydrodistention, 40% had intravesical therapy (drugs administered through the urethra), and 26% had urethral dilation (stretching of the urethra). Of these procedures, 24.4% to 45.3% of patients were improved by these procedures; whereas 27.0% to 49.8% felt no effect and 25.9% to 30.7% worsened. Of these surgical interventions, bladder instillations had the best-perceived outcome, deemed beneficial 45% of the time, although about one-quarter of respondents either reported that the treatment worsened their condition (28%) or resulted in no perceived effect (27%).
Comparatively, the majority of patients perceived that taking oral medications had improved their condition. The treatment with the greatest perceived benefit to patients? Taking an over-the-counter medication that neutralizes food acid. The authors concluded that medication therapy and other non-invasive procedures should be considered before invasive ones.
In 2017, the full data from 1628 patients were reanalyzed by a Canadian research team and published in the Journal of the Canadian Urological Association. They similarly found that oral medications had the greatest perceived benefit to patients; that a significant number of patients received treatments (like antibiotics) that are not recommended by guidelines; and some of the procedures recommended in the 2nd or 3rd line of treatment, such as intravesical medications and hydrodistention, had basically hurt patients as much as they helped.
2018;12(1):E1-5. http://dx.doi.org/10.5489/cuaj.4505
The authors wrote: “There is a disconnect between real-world patient perceived effectiveness of IC/BPS treatments compared to the efficacy reported from clinical trial data and subsequent guidelines developed from this efficacy data. Optimal therapy must include the best evidence from clinical research, but should also include real-life clinical practice implementation and effectiveness.” In other words, clinicians need to listen to patients about how they feel after treatments, and create treatment plans based on that feedback.
Why are invasive procedures overused?
Why have so many patients received invasive procedures for bladder pain and urgency? Zakariasen believes that financial incentives play a role, because reimbursements from insurers are greater for procedures than for discussing lifestyle changes or referring patients to physical therapy.
Zakariasen also thinks that doctors could do a much better job of informing patients about the benefits and harms of procedures. For example, patients may not be aware that the “procedure” that a urologist recommends is actually a surgery! Doctors often have the desire to “do something” to fix their patients’ problems, but this can cause unnecessary harm if they push patients into invasive treatments before discussing the evidence.
Before making a treatment recommendation, urologists should also talk to patients about their symptoms beyond just the bladder, to try and locate the underlying cause of pain. Zakariasen has interviewed dozens of patients who have found doctors who correctly diagnosed some of the many possible causes of pain, from allergies to viruses.
Zakariasen is trying to get the word out, to patients and doctors alike, to stop this form of iatrogenic harm. “Chronic pain caused by unnecessary surgeries and antibiotics takes the joy out of every moment of one’s life,” said Zakariasen. “This is a human rights issue.”
*For more on the harm caused by antibiotic overuse, Zakarian recommends the book Brain Maker by Dr. David Perlmutter and going to the website of the International Human Microbiome Consortium.
