The “deimplementation” process: Stopping overuse in pediatric care
Overuse in pediatrics is prevalent, but often goes overlooked. How can we improve health care value for people of all ages? In a recent viewpoint in JAMA Pediatrics, Dr. Elizabeth Wolf and Dr. Alex Krist from Virginia Commonwealth University, and Dr. Alan Schroeder from Stanford University argue that it is time for the field of pediatrics to develop their own pediatric “deimplementation science” to improve children’s health.
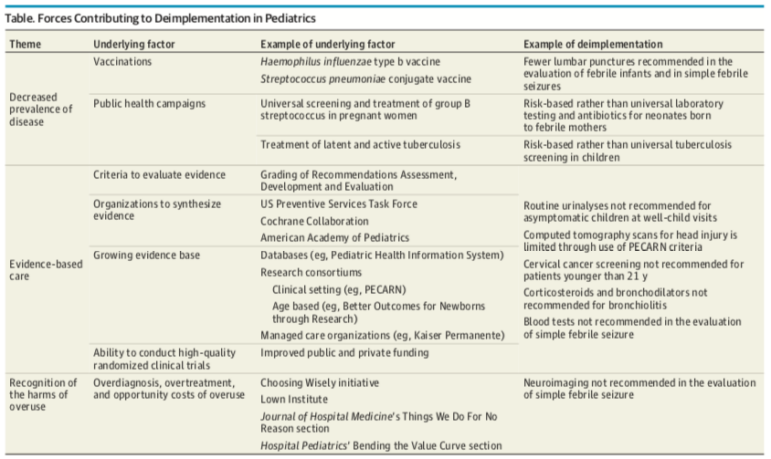
Deimplementation refers to “the process of reducing care that is harmful, ineffective, overused, or not cost-effective.” How do we “de-implement” harmful or unnecessary tests and procedures? The authors identify several forces that have driven reductions in low-value care in the recent past.
One is the decreased prevalence of childhood diseases through vaccination and public health campaigns; as more children are vaccinated, there is less need to test for certain diseases. Another is the rise of evidence-based pediatric care: the development of criteria to evaluate evidence, more funding for rigorous trials, and a growing evidence base around pediatric treatments. With more evidence comes the knowledge that some interventions are not as effective as we thought. And lastly, campaigns to raise awareness about the harms of low-value care have pushed clinicians and specialty groups to stop certain low-value services in pediatrics.
The authors acknowledge that there is still a long way to go toward “deimplementing” low-value services in children’s health. Despite changes in clinical guidelines, “there are many factors at the level of the patient (parental pressures, direct-to-consumer advertising), clinician (fear of missing a diagnosis, malpractice suits), and health care system (fee-for-service reimbursement, short visit times) that continue to drive pediatric overuse,” they write.
What changes do we need? Dr. Wolf says there are four main next steps: Developing benchmarks for low-value care for specific conditions, so that doctors can be evaluated on their progress; measuring the harms of overuse for children; understanding the best ways to stop each type of low-value care; and considering any potential unintended consequences of de-implementation.
This may be more difficult in pediatrics than in other fields, because acknowledging the harms of overuse has been slower in pediatrics, says Wolf. Historically, more attention has gone toward making sure that children receive care they need, like vaccines.
“There has been attention given to some examples of overuse, such as unnecessary treatment of bronchiolitis or antibiotics for upper respiratory infections, but very little attention given to other areas of overuse,” says Wolf.
However, pediatricians also recognize that because most children are healthy or just have an acute illness (rather than chronic conditions), the bar has to be higher to subject them to tests, medications, or other therapies than for adults for whom the prevalence of chronic conditions is much greater. Conducting more research on the potential harms of overuse in children and raising awareness should help pediatricians better understand which medical treatments clear that high bar– and which ones don’t.
