Are 3D mammograms better than none?
The U.S. Food and Drug Administration (FDA) approved digital breast tomosynthesis in 2011. This new technology is often known as a “3D mammogram,” because it creates a 3-dimensional image of breast tissue by taking x-rays through multiple tissue planes.
Studies have found that 3D mammograms detect more cancers than 2D mammograms and result in fewer false positives, which sounds great. However, there are some significant downsides to 3D mammograms. There have been no studies of whether or not using 3D mammograms actually improve morbidity, mortality, or quality of life. These scans may detect more cancers, but there isn’t evidence that the cancers being detected would have harmed patients, so 3D mammograms may also lead to more overdiagnosis and overtreatment. Even worse, older 3D mammograms expose women to more radiation than conventional 2D mammography. For all of these reasons, the US Preventive Task Force and the American Cancer Society state that there is not enough evidence to recommend 3D mammograms.
But the lack of evidence hasn’t stopped 3D mammograms from becoming incredibly popular in recent years. In one large study of privately insured women who received mammograms, use of 3D mammograms more than tripled in two years, from 12.9% of screening examinations in early 2015 to 43.2% in late 2017.
The rise of 3D likely has more to do with an intensive marketing process than evidence of benefit, writes Liz Szabo in a recent Kaiser Health News investigation. According to KHN’s analysis of Open Payments data, over the past 6 years, manufacturers of 3D mammogram equipment have paid doctors and teaching hospitals more than $9.2 million for research, speaking fees, consulting, and meals related to 3D mammograms.
Many clinicians who are spokespeople for 3D mammograms receive hundreds of thousands from companies that make this technology, yet they insist that this funding does not affect their opinion and they “can’t be bought.” Hologic, one of the largest manufacturers, has also funded specialty societies and patient advocate groups, and lobbied policymakers to have insurers cover the cost of 3D mammograms.
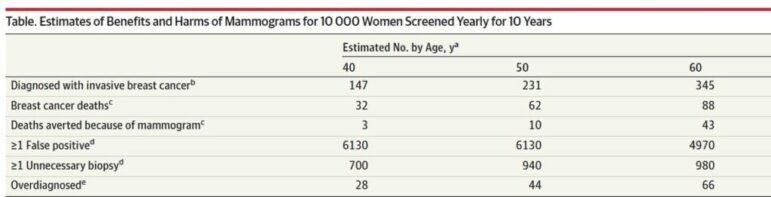
The rapid marketing push for 3D mammograms, followed by a corresponding increase in popularity of this technology, is disturbing given the lack of evidence that it saves any lives compared to 2D mammograms. Just as disturbing is the narrative that this marketing continues to push, that early detection of breast cancer is the best way to improve survival. As we’ve previously written, there has been little to no progress in reducing rates of mammography in low-risk women under 50, for which mammograms offer greater harms than benefits. Part of the problem is that most clinicians do not discuss the potential harms of overscreening for breast cancer, and most patients overestimate the benefits of screening as well.
The hype around 3D mammograms, condoned by the FDA and built by 3D equipment manufacturers, only hurts the problem more. When medical device manufacturers pay clinicians and advocacy groups to be cheerleaders for 3D, more patients hear the false message that new technology will find more cancers, and finding more cancers means saving more lives—without hearing anything about the potential harms of overdiagnosis.
